Medical Tourism is a Growing Trend
 Today’s short post features my response to a Forbes article by Dr. Robert Pearl, Offshoring American Health Care: Higher Quality At Lower Costs?, about the Cayman Islands, which are known for inviting coral-sand beaches, laid-back island culture and tax-free status.
Today’s short post features my response to a Forbes article by Dr. Robert Pearl, Offshoring American Health Care: Higher Quality At Lower Costs?, about the Cayman Islands, which are known for inviting coral-sand beaches, laid-back island culture and tax-free status.
Medical Tourism is a growing trend
This trend is not just in the Cayman Islands. Over 8 million people worldwide, and 1.3 million Americans, cross international borders for better and cheaper care. That trend will increase as insurers offer low-cost policies with high deductibles that encourage consumers to seek the best value in health care and lifestyle decisions.
There are many options for great care (Argentina, Brunei, Cuba, Colombia, Costa Rica, Honk Kong, Hungary, India, Jordan, Lithuania, Malaysia, The Philippines, Singapore, South Africa, Thailand, Saudi Arabia, UAE, South Korea, Tunisia, Ukraine). In Malaysia, for example, one can save 65-80% over the cost of having a procedure done here, and often the total cost, including airfare and 5-star hotel on the beach for recovery, is less than the annual insurance deductible.
The next trend is telehealth & telemedicine across state lines and international borders. Even though there’s a brewing States Right battle over licensure, this trend is unstoppable due to the Internet and easy ability for consumers to comparison shop and choose more affordable alternatives. All of this puts new pressure on the American healthcare system, which must innovate and adapt to compete. (See Fixing Health Care.)
Medical Tourism: Crossing Borders for Health Care
Infographic transcript follows for electronic screen readers…
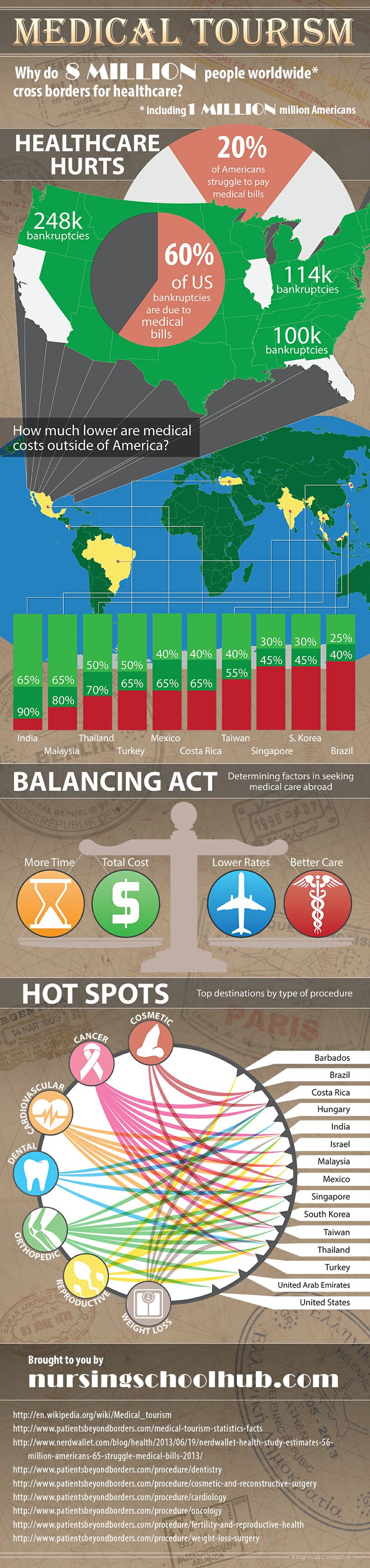
Why Would 8 million people cross borders for healthcare?
Including 1/300 in the U.S.?
20% of Americans struggle to pay medical bills
3 out of 5 bankruptcies are due to medical bills.
That’s 1.7 million Americans
Or 248,002 in California
113,524 in Illinois
and 99,780 in Florida alone.
Who could save…
India: 65-90%
Malaysia: 65-80%
Thailand: 50-70%
Turkey: 50-65%
Mexico: 40-65%
Costa Rica: 40-65%
Taiwan: 40-55%
Singapore: 30-45%
Korea: 30-45%
Brazil: 25-40%
Over U.S. prices for the same medical procedures.
Things to Balance
High Wait Times
High Costs
High Quality Care in Many Nations
Low Cost of International Travel
But what about…
Airfare:
1980: $1029
2012: $926
…And it’s set to fall farther
Recovery:
Often it goes like this:
Flight -> Pre-procedure care nursing -> Procedure ->Post-procedure care nursing -> Flight home.
And there are so many options:
Argentina, Brunei, Cuba, Colombia, Costa Rica, Honk Kong, Hungary, India, Jordan, Lithuania, Malaysia, The Philippines, Singapore, South Africa, Thailand, Saudi Arabia, UAE, South Korea, Tunisia, Ukraine
And specialties
1.) Cosmetic Surgery
Most cosmetic surgery is not covered by insurance.
Most popular destinations:
Worldwide:
Rio de Janeiro, Brazil
Chang-Gung Memrial Hospital in Taoyuan, Taiwan
For Americans:
Costa Rica
Mexico
2.) Dentistry
Nearly half of Americans have no dental coverage.
Most popular locations:
Right across borders:
Americans –> Mexico, Costa Rica
Europeans –> Hungary
Asians –> Thailand
Top Hospitals:
Bumrungrad in Bangkok, Thailand
and Hospital San Jose Tec de Monterrey in Mexico.
3.) Cardiovascular
Cardiovascular disease is the number one killer in Europe, and 16.7 million die yearly worldwide from CVD. This leaves experienced CVD doctors worldwide to cater to medical tourists.
Most popular locations:
Mexico, India, Malaysia, Taiwan, Singapore, Turkey, Thailand, Korea.
Top Destinations:
Wockhardt Heart Hospitals in Bangalore, Mumbai, and Nagpur India.
4.) Orthopedics
More than 20% of Americans have arthritis, with 2/3 under 65. With better prostheses, and prices up to 80% lower than in the states, orthopedic surgery is a good reason to be a medical tourist.
Most Popular Destinations:
Bangkok, Thailand
San Jose, Costa Rica
Bangelore and New Delhi, India
Seoul, South Korea
Mayo Clinic, Minnesota
Malaysia
Monterrey, Mexico
Singapore
Taiwan
Dubai, UAE
5.) Cancer
Cancer is the second leading killer in the developed world, and treatment is often prohibitively expensive.
Top Destinations:
Turkey, Singapore
Other Destinations:
Seoul, South Korea
Sao Paulo, Brazil
San Jose, Costa Rica
Delhi, Bangalore, Mumbai, India
Petah Tikva, Israel
Malaysia
Singapore
Monterrey, Mexico
Taiwan
6.) Reproductive
One in six couples fall under the “infertile” designation, but reproductive healthcare can be prohibitively expensive.
Top Destinations:
Barbados, Israel
Other Destinations:
Mumbai, New Delhi, India
Malaysia
Bangkok, Thailand
Dubai, UAE
7.) Weight Loss
2.5 million people die of obesity associated deaths yearly, and the annual healthcare bill is massive. Bariatric surgeries cost $20-$25,000 in the U.S., but half that abroad.
Top Destinations:
Malaysia
Sao Paulo, Brazil
San Jose, Costa Rica
Mumbai, New Delhi, Bangalore, India
Taiwan
Monterrey, Mexico
Bangkok, Thailand
Joint Commission International (JCI) accreditation for hospitals and individual doctors is a good indicator of developed world quality healthcare, wherever it is.
Citations:
- Wikipedia, Medical Tourism
- Patients Beyond Borders Stats
- Nerd Wallet On Medical Expenses
- Patients Without Borders, Dentistry
- Patients Without Borders, Cosmetic Surgery
- Patients Without Borders, Cardiovascular
- Patients Without Borders, Oncology
- Patients Without Borders, Fertility and Reproductive Health
- Patients Without Borders, Weight Loss Surgery

Nice article keep it up !!
ivf cost in delhi, ivf cost in india
ivf doctor in delhi
ivf cost in delhi, ivf cost in india
ivf doctor in delhi
Medical tourism is growing, yes it is true. Lots of individuals opt for it because they can find it as one of their best solution. The article is so great and informative. If you want to know more information, you can visit http://www.medicaltourism-guide.com/.
RELATED ARTICLES:
This article lists resources describing in-bound and out-bound medical tourism and where the hot-spots are: http://www.1ohww.org/business-inbound-medical-tourism/
Walmart is so desperate to fix health care, it flies employees to top hospitals in other states for treatment (CNBC, March 2019)